Apollo Medical Holdings Investor Presentation Deck
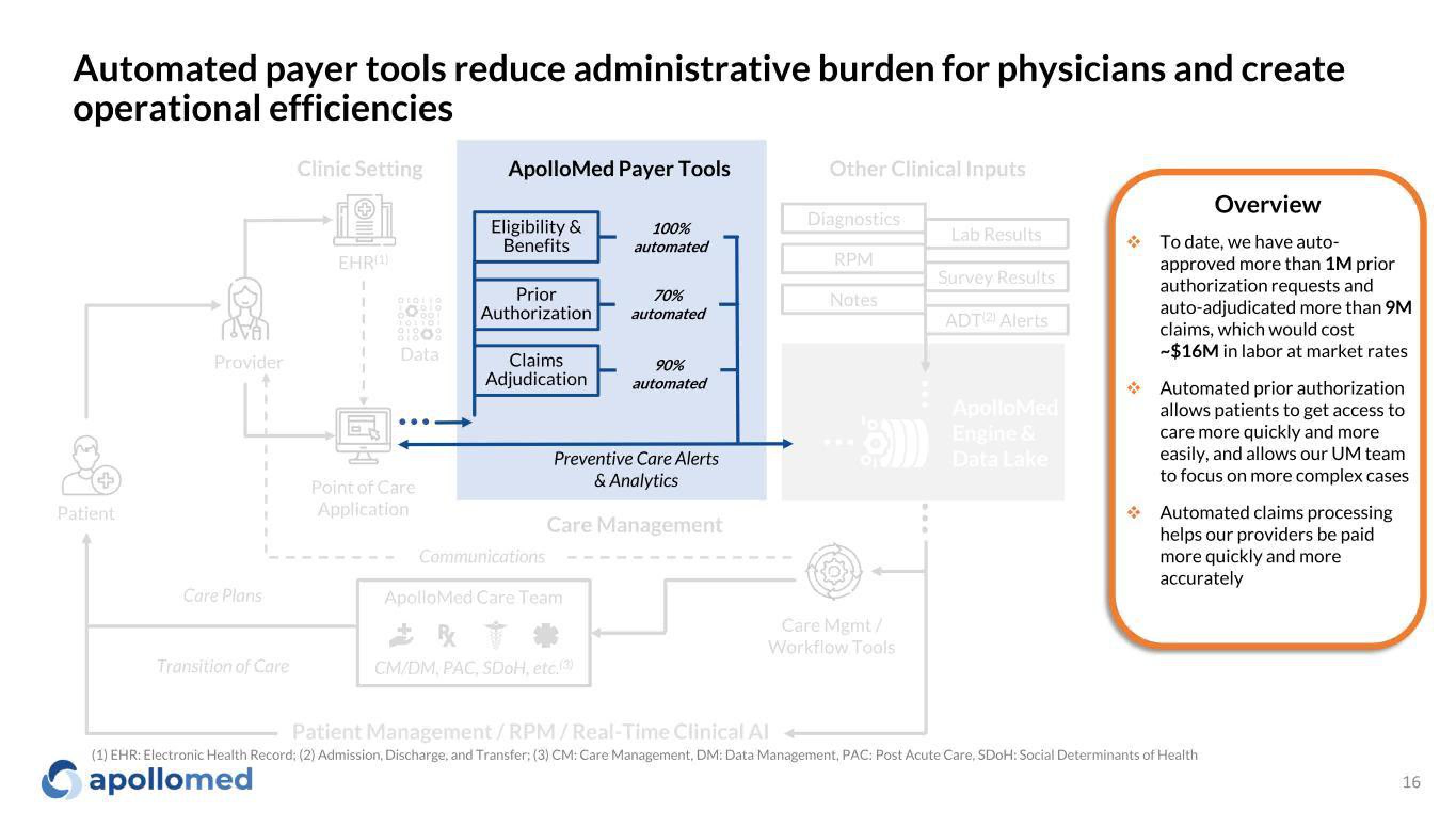
Automated payer tools reduce administrative burden for physicians and create
operational efficiencies
Patient
Provider
I
T
Care Plans
Transition of Care
Clinic Setting
1ºh
EHR(¹)
I
Data
Point of Care
Application
ApolloMed Payer Tools
Eligibility &
Benefits
Prior
Authorization
Claims
Adjudication
100%
automated
Communications
ApolloMed Care Team
B
CM/DM, PAC, SDOH, etc.(3)
70%
automated
90%
automated
Preventive Care Alerts
& Analytics
Care Management
Other Clinical Inputs
Diagnostics
RPM
Notes
Care Mgmt /
Workflow Tools
Lab Results
Survey Results
ADT Alerts
ApolloMed
Engine &
Data Lake
Overview
To date, we have auto-
approved more than 1M prior
authorization requests and
auto-adjudicated more than 9M
claims, which would cost
-$16M in labor at market rates
Automated prior authorization
allows patients to get access to
care more quickly and more
easily, and allows our UM team
to focus on more complex cases
Automated claims processing
helps our providers be paid
more quickly and more
accurately
Patient Management/RPM/Real-Time Clinical Al
(1) EHR: Electronic Health Record; (2) Admission, Discharge, and Transfer; (3) CM: Care Management, DM: Data Management, PAC: Post Acute Care, SDOH: Social Determinants of Health
apollomed
16View entire presentation