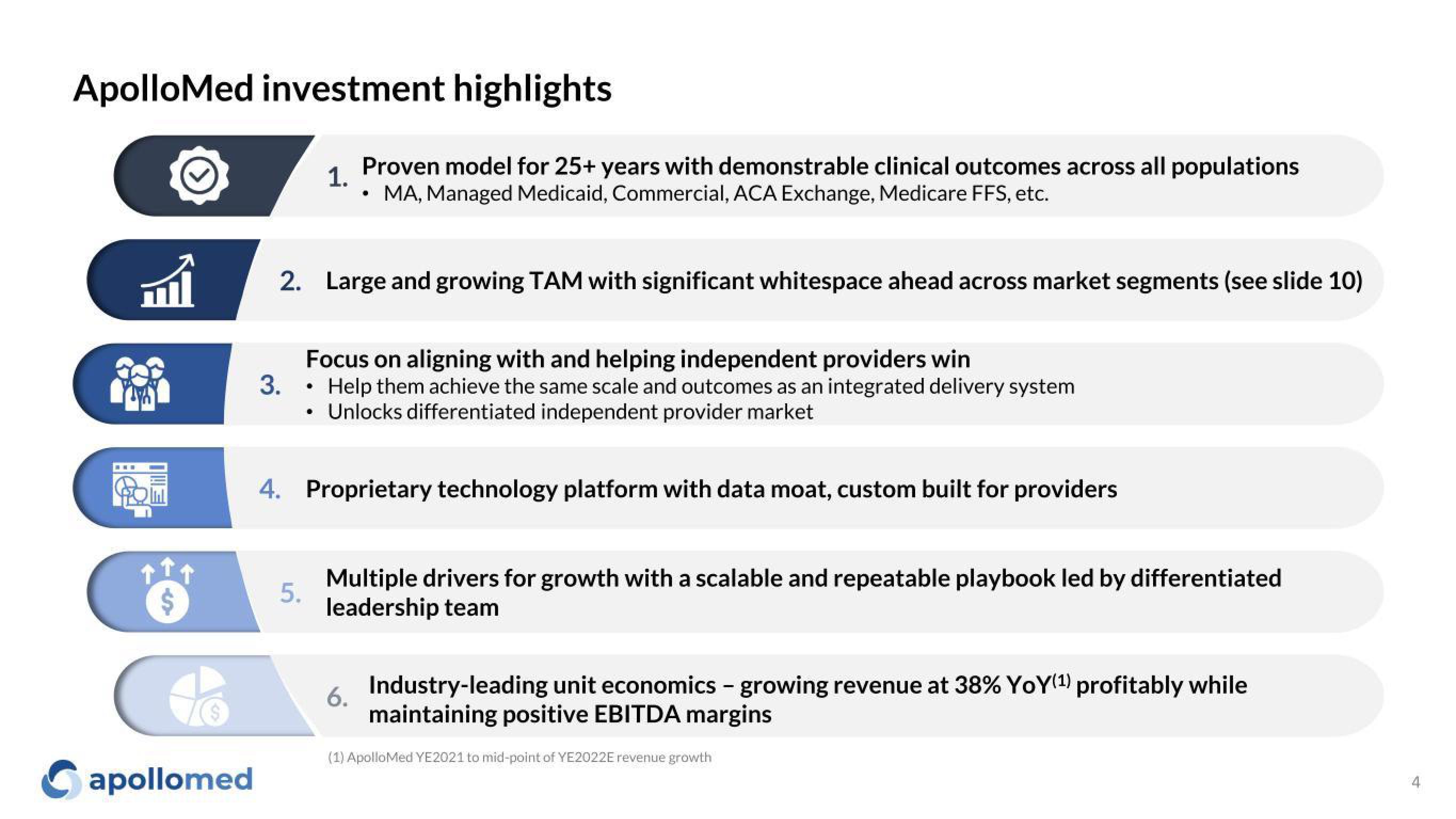
Apollo Medical Holdings Investor Presentation Deck
Made public by
Apollo Medical Holdings
sourced by PitchSend
Creator
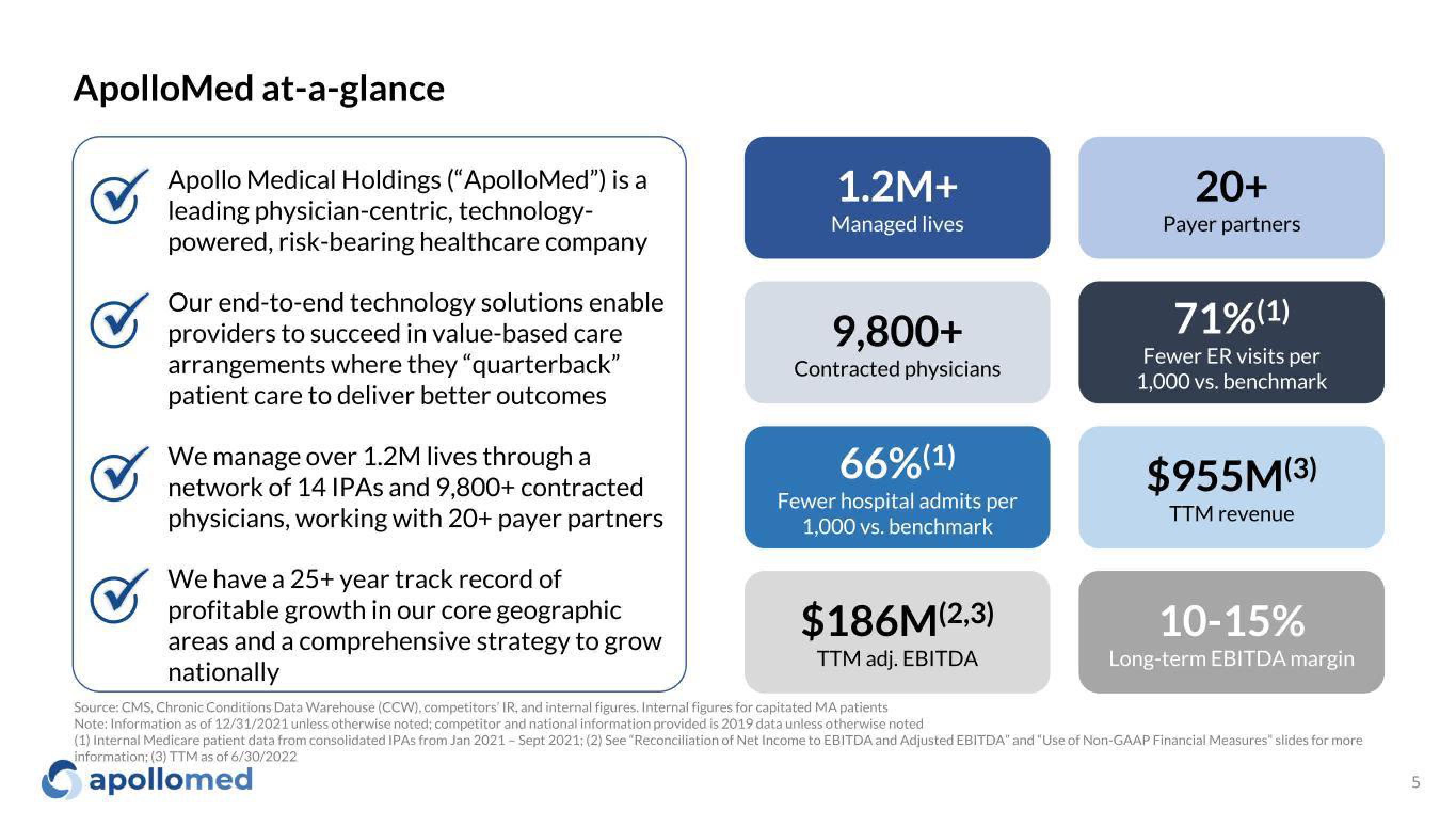
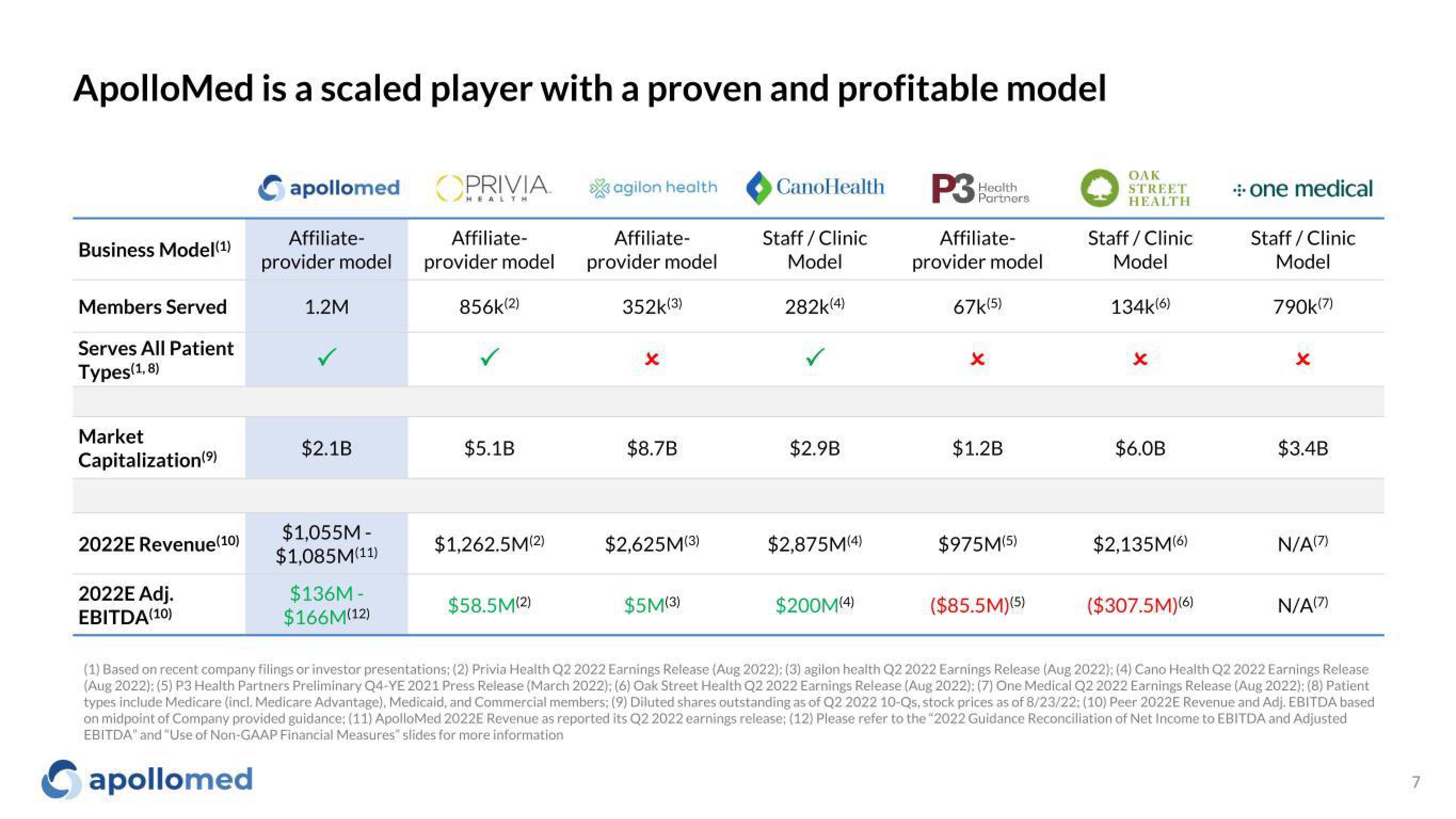
apollo-medical-holdings
Category
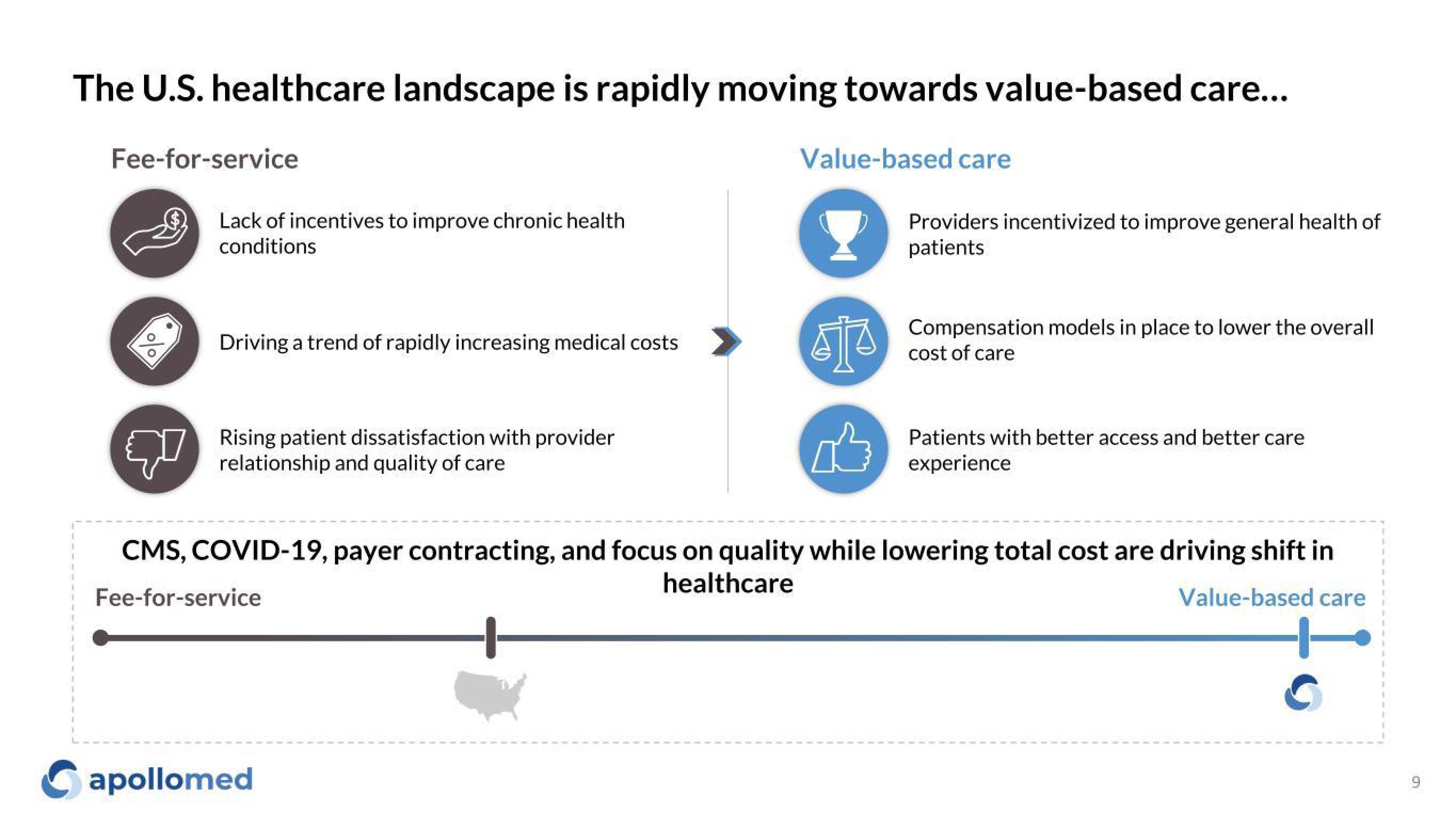
Healthcare
Published
October 2022
Slides
Transcriptions
Download to PowerPoint
Download presentation as an editable powerpoint.
Related